As the novel coronavirus spreads across the United States, the number of individuals suffering from pneumonia and flu-like symptoms caused by the disease is set to dramatically rise. With this in mind, now is a good time to ask whether the US health care system is up to the task.
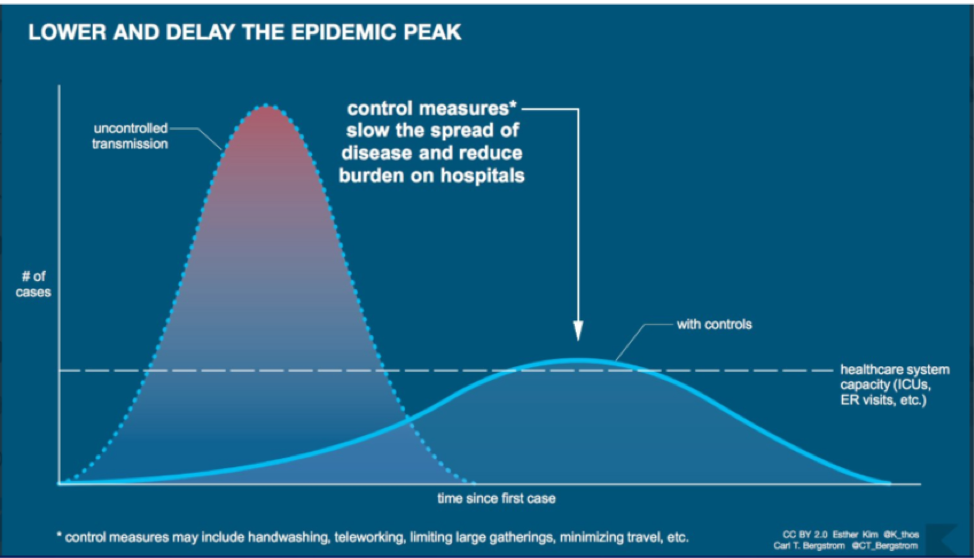
Italy experienced a surge in demand for health services far in excess of what it was able to supply after failing to effectively manage the virus’s spread. Their inadequate supply of ventilator machines, which help move air into the lungs of patients that have difficulty breathing, proved particularly problematic. The shortage forced Italy to make hard choices regarding the use of limited resources, resulting in more deaths than would have otherwise occurred if the virus had spread at a slower rate. Indeed, the mortality rate associated with COVID-19 rises substantially when health system systems become overwhelmed, as illustrated in the graphic below.
Is the United States similarly ill-prepared?
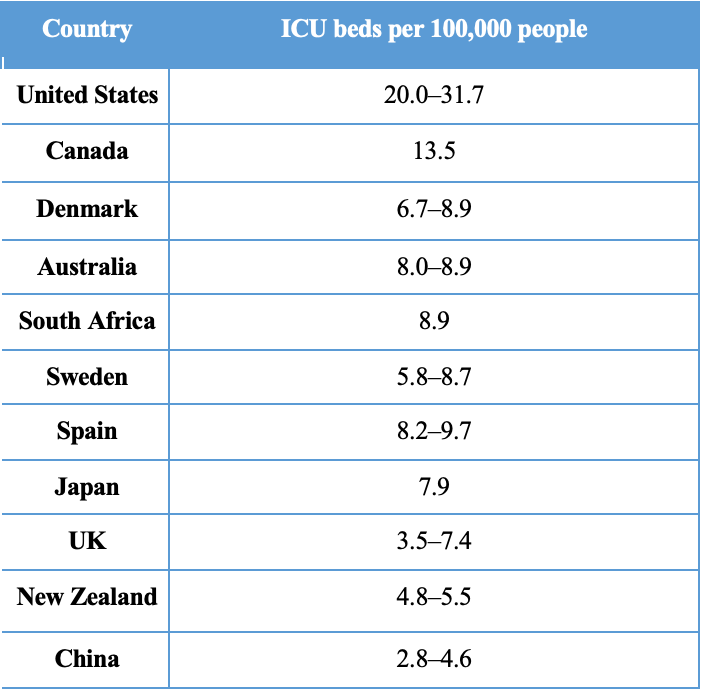
One encouraging sign for the United States is our high number of intensive care unit (ICU) beds per person. The density of ICU beds is a significant indicator of coronavirus preparedness because ICU beds are typically equipped with ventilator machines, which are lifesaving in cases of respiratory illnesses such as COVID-19. Even compared with similarly wealthy countries, the number of ICU beds per person in the United States is exceptionally high.
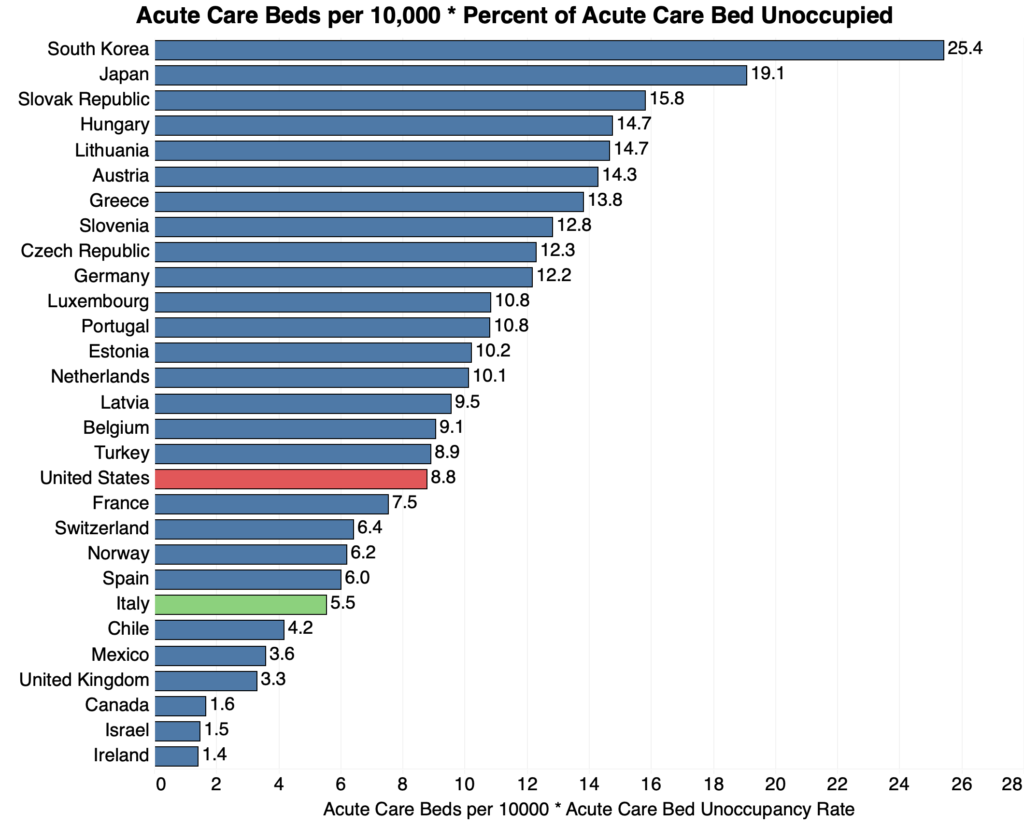
Some have suggested that total hospital beds per-capita is also an important indicator of a country’s response capacity. The OECD gives the United States a relatively low score on its measure of total hospital beds, suggesting the United States may be ill-prepared compared to other rich countries. The intuition here is that the virus necessitates triaging resources from elsewhere in the health system, and the United States looks poorly prepared to do so.
Fortunately, the OECD’s density of total hospital beds statistic understates the US’s preparedness in at least three ways. First, and most importantly, the density of all hospital beds says little about whether such beds are equipped with the ventilators necessary to deal with respiratory illness. Second, the total hospital beds statistic includes facilities dedicated to long-term or psychiatric care, which are likely of limited use during a viral outbreak. Finally, the total number of beds does not capture the excess capacity that can be rapidly devoted to coronavirus response.
Breaking out the density of beds devoted to acute care from the OECD’s total provides a clearer picture of the intensive care (ICU) and intermediate care (IMCU) hospital beds that are most useful during an outbreak. While ventilator-equipped ICU beds will be most crucial, IMCUs can play a useful secondary role by allowing for coordinated monitoring of patients who may develop severe symptoms. An estimate of the excess bed capacity that can be devoted to coronavirus response in the United States can be produced by combining the density of acute care beds with their utilization rate. When the type of hospital bed and pre-existing level of utilization are accounted for, the US has significantly more acute care beds available for patients than Italy, although many fewer than South Korea. In fact, Korea has far more acute care bed capacity than any other OECD country, which may be a factor behind their success in reducing COVID-19’s lethality.
US Workforce Limitations Pose Greatest Risk
While the US benefits in terms of disaster-preparedness as a consequence of heavy investments in high-intensity health care services such as ICU beds and ventilators, there are other margins where we risk falling short. A lack of appropriately-trained staff able to manage and provide the necessary care is more likely to be our limiting factor than fixed-cost supplies. Studies find that mass emergency care often requires scaling up the medical workforce to such an extent that it may prove difficult in the US. And improper ventilator usage can result in serious complications if operated by untrained hands.
The physician workforce of the United States is smaller than in most rich countries. This may make it more difficult to reallocate physician capacity toward the treatment of COVID-19 than in other countries. Policies that increase the practice authority of nurse practitioners and physician assistants are therefore a promising strategy for bolstering disaster-preparedness.
The United States is likely better prepared for the coronavirus than was Italy. The United States health care system has invested heavily in high-intensity medical care including ventilators and ICUs, which should make a breakdown in treatment less likely. The much more worrying bottleneck is simply the insufficient supply of skilled staff in the face of emergency levels of demand. In addition to slowing the rate of infection, public officials should consider actions designed to expand the supply of health care workers, from liberalizing licensure requirements to expediting licenses for practitioners from out of state.